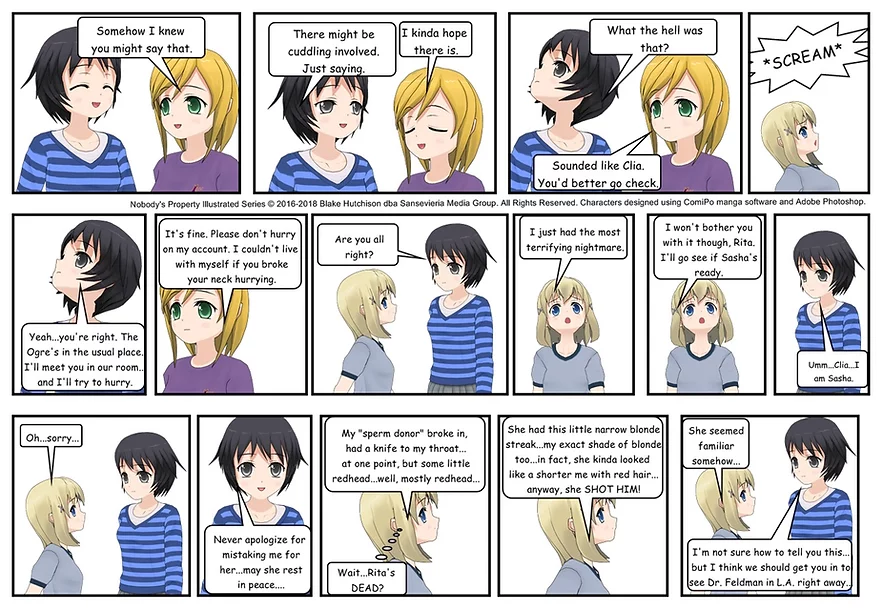
Nobody's Property Illustrated Series #27
Previous... ...Next
Previous... ...Next
Where to buy CBD
There is evidence to suggest that a traumatic brain injury (TBI) can potentially increase the risk of developing schizophrenia or trigger symptoms similar to those seen in schizophrenia. Traumatic brain injuries are caused by severe head trauma, such as a blow or jolt to the head, and can lead to various cognitive, emotional, and behavioral changes.
Research has shown that individuals who have experienced a traumatic brain injury, especially more severe cases, may have an increased risk of developing psychiatric disorders, including schizophrenia. The exact mechanisms by which traumatic brain injury, like Nadia’s mom Clia sustained as a result of being pushed down a flight of stairs at a young age, and schizophrenia, which she also was diagnosed with as a teenager, are connected are not fully understood, but it is believed that the physical damage to the brain, disruption of neural circuits, and changes in neurotransmitter function may contribute to the development of psychotic symptoms.
It is important to note that not everyone who experiences a traumatic brain injury will develop schizophrenia. Traumatic brain injury cases can have a wide range of effects depending on the severity, location, and individual factors. While there may be an increased risk, the development of schizophrenia after a traumatic brain injury is relatively rare.
If someone experiences a traumatic brain injury and later develops symptoms resembling schizophrenia, it is crucial to consult with a healthcare professional who can conduct a thorough evaluation and provide appropriate diagnosis and treatment. Proper assessment and management of both the TBI and the potential psychiatric symptoms are essential for the individual's overall well-being and recovery.
Schizophrenia is a chronic and complex mental disorder that affects how a person thinks, feels, and behaves. It is characterized by a range of symptoms that can significantly impact an individual's daily life and relationships. While schizophrenia is relatively rare, it can be a lifelong condition that requires ongoing management and support.
The hallmark symptoms of schizophrenia are classified into positive, negative, and cognitive categories. Positive symptoms include hallucinations (perceiving things that aren't there) and delusions (holding false beliefs). Negative symptoms involve a loss of normal functions, such as reduced motivation, social withdrawal, and a limited range of emotions. Cognitive symptoms can affect memory, attention, and problem-solving abilities.
The exact causes of schizophrenia remain unknown, but a combination of genetic, environmental, and neurological factors are believed to contribute to its development. Research suggests that imbalances in brain chemistry and abnormalities in brain structure may play a role. Stressful life events, substance abuse, and a family history of schizophrenia can also increase the risk of developing the disorder.
Treatment for schizophrenia typically involves a combination of medication, therapy, and support services. Antipsychotic medications can help manage the symptoms by reducing hallucinations, delusions, and emotional instability. Psychotherapy, such as cognitive-behavioral therapy, can assist individuals in managing their thoughts, coping with stress, and improving social skills. Additionally, support from family, friends, and mental health professionals is crucial in helping individuals with schizophrenia lead fulfilling lives and achieve their goals.
Nobody's Property is published by Sansevieria Media. All Rights Reserved.
© Nobody's Property Illustrated Series, copyright 2018- | all rights reserved. This illustrated series is for entertainment purposes only. Please do not attempt any homicidal, vigilante, or other illegal acts.